Research partnership to fast-track Myovolt for stroke rehabilitation.
Announcing our collaboration with leading experts in neurotechnology at University of Hertfordshire, UK.
Research partnership to fast-track Myovolt for stroke rehabilitation.
Announcing our collaboration with leading experts in Neurotechnology at University of Herfordshire, UK.
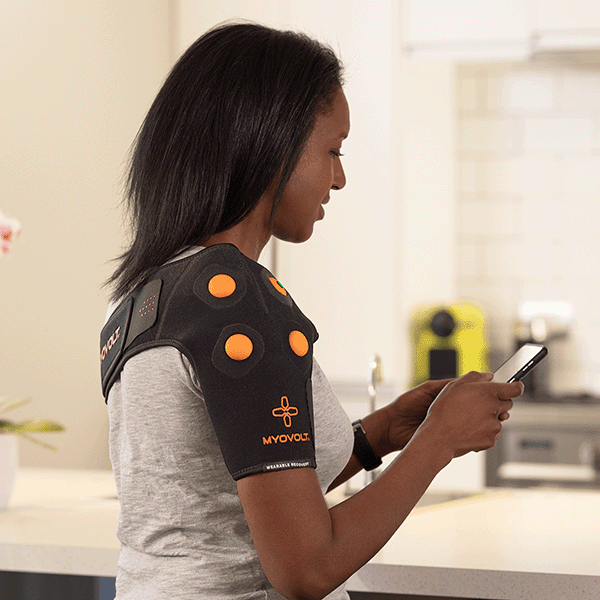
Myovolt has joined forces with the University of Hertfordshire in the UK to tackle a significant challenge in the global rehabilitation market. Together, we are developing innovative wearable technology to improve the functional mobility of millions of people living with disabilities caused by neurological conditions such as stroke and cerebral palsy or brain and spinal cord injury.
The collaboration is spearheaded by leading expert Associate Professor Amit Pujari, who is a distinguished Fellow of the Royal Academy of Engineering and recognised as one of emerging healthcare research leaders by the Academy of Medical Sciences, UK.
The partnership with Myovolt will accelerate the development of next-generation wearable therapeutic devices that provide remote rehabilitation treatment in the home. The technology delivers clinically directed Focal Vibration Therapy via comfortable, ultrathin garments that can be worn on upper and lower limbs. This is a drug-free neuromuscular treatment to reduce muscle spasticity and improve functional movement, helping people perform activities of daily living and retain their independence.
Neurological conditions that cause spasticity are on the rise globally with stroke now impacting over 1.3 million people in the UK alone.
“This technology offers the potential to change the way rehabilitation treatment is delivered over the long term for these disabling conditions’ says Dr Pujari.
Dr Pujari's team is currently conducting clinical trials with stroke patients at the pioneering rehabilitation clinic Hobbs Rehabilitation in the UK. Initial results were presented at the MiNT 24 conference on 15th April at the Royal Society of Medicine in London [ 1 ]. This event is a forum for leading researchers in the fields of neurotechnology and rehabilitation therapy.
Clinical trials will be expanded in the UK mid 2024 in partnership with Leeds Teaching Hospitals with a focus on validating the technology and ease of use for patient recovery in the home. In parallel, commercialisation work is being fast-tracked with a target of products in market and available for patient use as early as 2025.
“The aim is to make our wearable therapeutic device the most effective and user-friendly solution for spasticity reduction available” says Dr Dianne Jones of Myovolt. “We believe technology can revolutionize the delivery rehabilitation treatment. If therapy is made more accessible and convenient, people will be able to manage the severity of symptoms and support their own recovery over extended periods.”
This innovative technology combines treatment and functional performance measurement enabling clinicians to monitor the progress of recovery and ultimately provide personalised rehabilitation tailored to an individual's needs and daily routines.
Stay tuned for further updates on clinical trials and the progress of this groundbreaking collaboration.
Dr. Amit Pujari is a world-leading biomedical engineer and neuroscientist who researches medical device development and neurophysiology. A Senior Lecturer at the University of Hertfordshire, Dr. Pujari was recently announced as a recipient of the prestigious Royal Academy of Engineering/Leverhulme Trust Research Fellowship.
Dr. Amit Pujari is a world-leading biomedical engineer and neuroscientist who researches medical device development and neurophysiology. A Senior Lecturer at the University of Hertfordshire, Dr. Pujari was recently announced as a recipient of the prestigious Royal Academy of Engineering Leverhulme Trust Research Fellowship.
More about stroke and muscle spasticity.
Stroke is one of the major causes of mortality and disability across the world with over 12.2 million new strokes each year and 6.5 million deaths. One in four people over age 25 will have a stroke in their lifetime and 101 million people worldwide are currently living with the aftermath of stroke with this figure having doubled over the last 30 years. With a global cost of $721 billion per year, stroke is the third leading cause of years of life lost and of disability adjusted life years [ 2 ].
Following stroke, 50% of people have upper-limb motor disability and around 40-50% have spasticity which is disabling muscle stiffness. This severe muscle stiffness and tightness is due to prolonged muscle contraction preventing completion of the full range of motion. Also called muscle tone it can impair movement and prevent actions such as releasing a grasp and performing activities-of-daily-living (e.g. eating, drinking, buttoning a shirt). The degree of spasticity can range from mild muscle stiffness to severe, painful, and uncontrollable muscle spasms.
Spasticity commonly affects muscles in upper and lower limbs and impairs the functional mobility of the elbow, wrist and ankle. If spasticity is left untreated it can lead to prolonged involuntary muscle contraction that causes joints in the leg or arm to become frozen in abnormal and painful positions.
Spasticity is generally caused by damage to nerve pathways within the brain or spinal cord that control muscle movement. It is a symptom associated with damage to the brain, spinal cord or motor nerves and is seen in individuals with neurological conditions, such as Stroke, Multiple Sclerosis, Cerebral Palsy or spinal cord and brain injury.
Current treatments include physical therapy to stretch and strengthen muscles and improve range of motion. Oral medications such as baclofen and tizanidine are used as muscle relaxants but cause drowsiness and other side effects. Botox injections to selectively disable high tone muscles to improve movement, but the effect is short-term and there are dosage limits. In severe cases surgery may be performed for tendon release or to sever the nerve-muscle pathway.
References
1.
MiNT UK 24 https://themintacademy.co.uk/mint-uk-2024
2. World Stroke Organisation Fact Sheet 2022 https://www.world-stroke.org/news-and-blog/news/wso-global-stroke-fact-sheet-2022